Location
The thyroid gland is placed anteriorly in the lower neck, level with the fifth cervical to the first thoracic vertebrae.
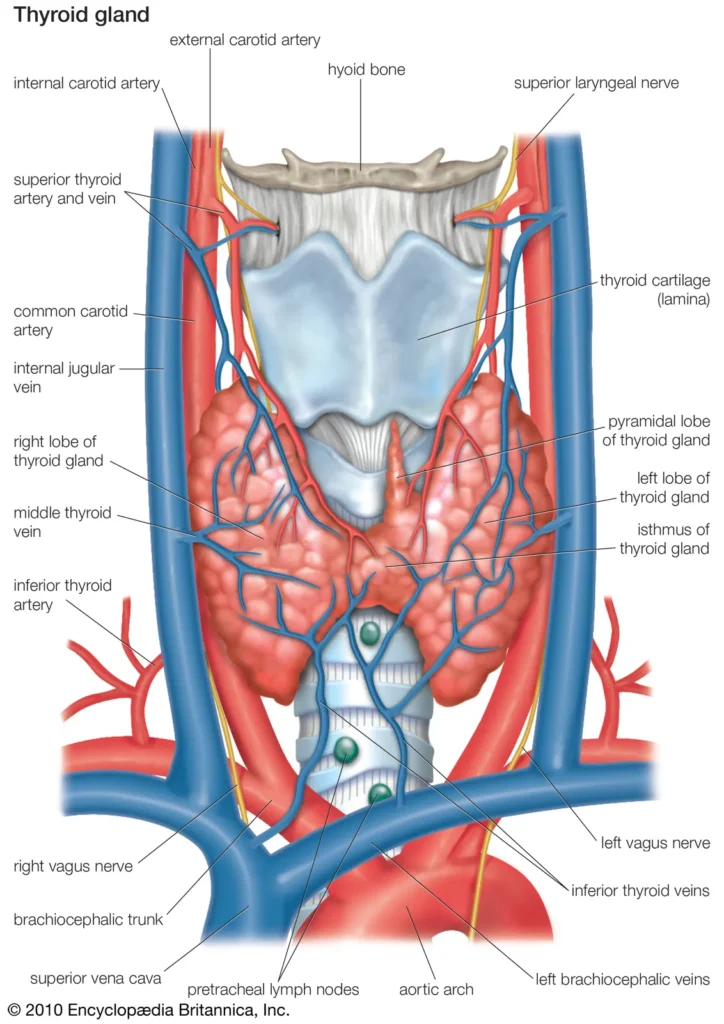
Appearance
The thyroid gland is brownishred and highly vascular. It is ensheathed by the pre-tracheal layer of deep cervical fascia and consists of right and left lobes connected by a narrow, median isthmus. It usually weighs 25 g but this varies. The gland is slightly heavier in females and enlarges during menstruation and pregnancy. The lobes of the thyroid gland are approximately conical.
Anatomy
Their ascending apices diverge laterally to the level of the oblique lines on the laminae of the thyroid cartilage, and their bases are level with the fourth or fifth tracheal cartilages. Each lobe is usually 5 cm long, its greatest transverse and anteroposterior extents being 3 cm and 2 cm, respectively. The posteromedial aspects of the lobes are attached to the side of the cricoid cartilage by a lateral thyroid ligament (Berry’s ligament). The isthmus connects the lower parts of the two lobes, although occasionally it may be absent. It measures 1.25 cm transversely and vertically and is usually anterior to the second and third tracheal cartilages. However, it can be higher or sometimes lower because its site and size vary greatly. A conical pyramidal lobe often ascends towards the hyoid bone from the isthmus or the adjacent part of either lobe (more often the left). It is occasionally detached or in two or more parts. A fibrous or fibromuscular band, the levator of the thyroid gland, musculus levator glandular thyroid, sometimes descends from the body of the hyoid to the isthmus or pyramidal lobe.
Surfaces and relations
The convex lateral (superficial) surface is covered by the sternothyroid, whose attachment to the oblique thyroid line prevents the upper pole of the gland from extending onto the thyrohyoid. More anteriorly lie the sternohyoid and the superior belly of the omohyoid, overlapped inferiorly by the anterior border of the sternocleidomastoid. The medial surface of the gland is adapted to the larynx and trachea; its superior pole contacts the inferior pharyngeal constrictor and the posterior part of cricothyroid, which separate it from the posterior part of the thyroid lamina and the side of the cricoid cartilage. The external branch of the superior laryngeal nerve is medial to this part of the gland as it passes to supply cricothyroid. Inferiorly, the trachea and, more posteriorly, the recurrent laryngeal nerve and oesophagus (which is closer on the left) are medial relations. The posterolateral surface of the thyroid gland is close to the carotid sheath and overlaps the common carotid artery.
The anterior border of the gland is thin, and near the anterior branch of the superior thyroid artery, it slants down medially. The posterior border is rounded and related inferiorly to the inferior thyroid artery and its anastomosis with the posterior branch of the superior thyroid artery. On the left side, the lower end of the posterior border lies near the thoracic duct. The parathyroid glands are usually related to the posterior border.
The isthmus is covered by sternothyroid, from which it is separated by pre-tracheal fascia. More superficially it is covered by the sternohyoid, the anterior jugular veins, the fascia and the skin. The superior thyroid arteries anastomose along its upper border and the inferior thyroid veins leave the gland at its lower border.
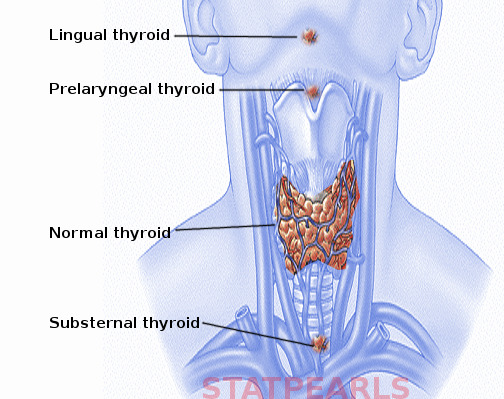
Clinical Correlations
Ectopic thyroid tissue is rare but may be found around the course of the thyroglossal duct or laterally in the neck and distant places such as the tongue (lingual thyroid), mediastinum and the subdiaphragmatic organs. The most frequent location of ectopic thyroid tissue is at the base of the tongue, particularly at the region of the foramen caecum; it is often the only thyroid tissue present. Small, detached masses of thyroid tissue may occur above the lobes or isthmus as accessory thyroid glands. Vestiges of the thyroglossal duct may persist between the isthmus and the foramen caecum of the tongue, sometimes as accessory nodules or cysts of thyroid tissue near the midline or even in the tongue, where they are called thyroglossal duct cysts.
Vascular supply and lymphatic drainage
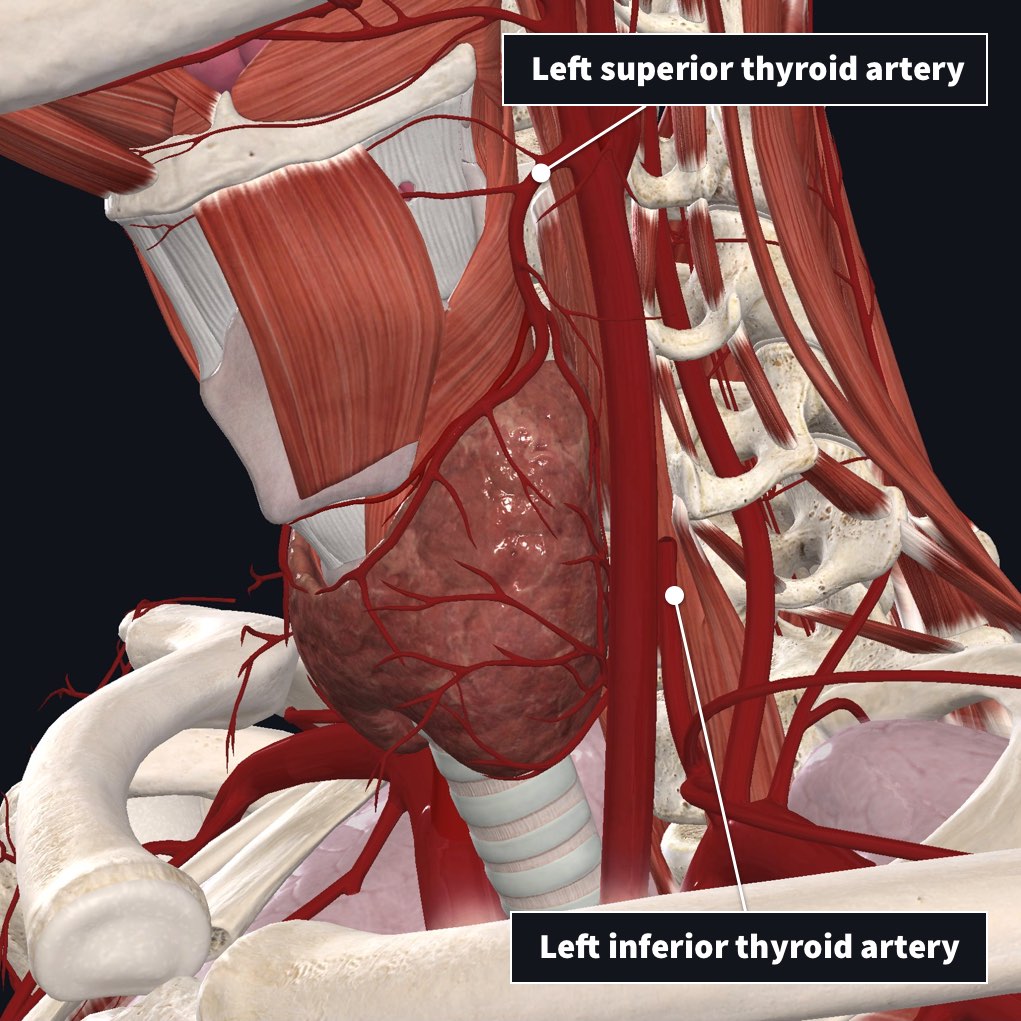
Arteries
The superior and inferior thyroid arteries supply the thyroid gland and sometimes an arteria thyroidea from the brachiocephalic trunk or aortic arch. The arteries are large and their branches frequently anastomose both on and in the gland, ipsilaterally and contralaterally. The superior thyroid artery, closely related to the external branch of the superior laryngeal nerve, pierces the thyroid fascia and then divides into anterior and posterior branches.
The anterior branch supplies the anterior surface of the gland, and the posterior branch supplies the lateral and medial surfaces. The inferior thyroid artery approaches the base of the thyroid gland and divides into superior (ascending) and inferior thyroid branches supplying the gland’s inferior and posterior surfaces. The superior branch also supplies the parathyroid glands. The relationship between the inferior thyroid artery and the recurrent laryngeal nerve is highly variable and of considerable clinical importance; iatrogenic injury to the nerves that supply the larynx represents a major complication of thyroid surgery. The recurrent laryngeal nerve is usually related to the posterior branch of the inferior thyroid artery, which a vascular network may replace.
Veins
The venous drainage of the thyroid gland is usually via superior, middle and inferior thyroid veins. The superior thyroid vein emerges from the upper part of the gland and runs with the superior thyroid artery towards the carotid sheath; it drains into the internal jugular vein. The middle thyroid vein collects blood from the lower part of the gland; it emerges from the lateral surface of the gland and drains into the internal jugular vein. The inferior thyroid veins arise in a glandular venous plexus, which also connects with the middle and superior thyroid veins. These veins form a pre-tracheal plexus, from which the left inferior vein descends to join the left brachiocephalic vein, and the right descends obliquely across the brachiocephalic artery to join the right brachiocephalic vein at its junction with the superior vena cava. The inferior thyroid veins often open via a common trunk into the superior vena cava or left brachiocephalic vein. They drain the oesophageal, tracheal and inferior laryngeal veins and have valves at their terminations.
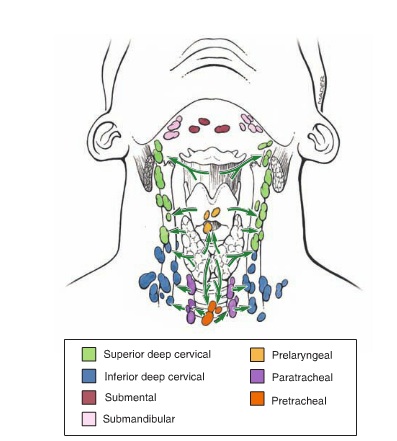
Lymphatics
Thyroid lymphatic vessels communicate with the tracheal plexus, and pass to the prelaryngeal nodes just above the thyroid isthmus and the pretracheal and paratracheal nodes; some may also drain into the brachiocephalic nodes related to the thymus in the superior mediastinum. Laterally, the gland is drained by vessels lying along the superior thyroid veins to the deep cervical nodes. Thyroid lymphatics may drain directly, with no intervening node, to the thoracic duct.
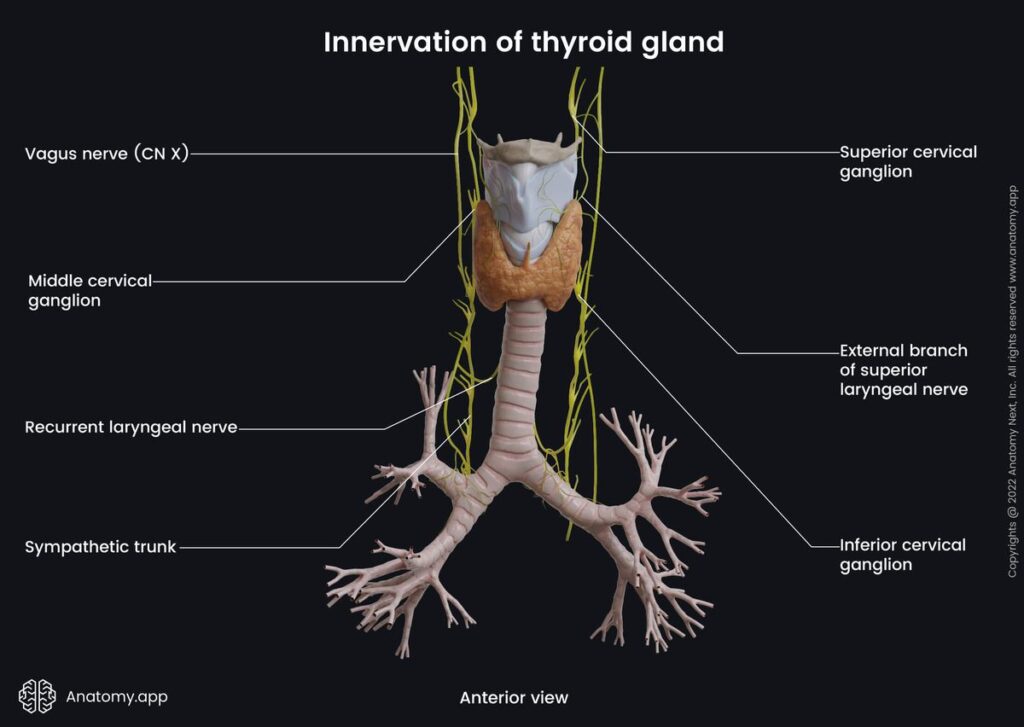
Innervation
The thyroid gland receives its innervation from the superior, middle and inferior cervical sympathetic ganglia. Postganglionic fibres from the inferior cervical ganglion form a plexus on the inferior thyroid artery, which accompanies the artery to the thyroid gland, and communicates with the recurrent laryngeal and external branch of the superior laryngeal nerves, with the superior cardiac nerve, and with the plexus on the common carotid artery.
Imaging
The follicular nature of the thyroid gland is not resolved by current imaging techniques and thus presents a homogeneous texture on cross-sectional imaging (ultrasound, computed tomography, magnetic resonance imaging (MRI)). Its superficial location makes the thyroid an ideal organ for sonographic examination. The thyroid gland is highly vascular and demonstrates intense contrast enhancement and increased signal on T2-weighted MRI (Fig. 29.22). Radionuclide imaging of the thyroid may be performed with technetium (99mTc) pertechnetate. This readily available radionuclide is trapped by the thyroid in the same way as iodine but is not organised. It yields morphological information and will reveal the presence of ectopic thyroid tissue. Functional data can be obtained with the use of 123iodine or 131iodine, which is trapped and organified.
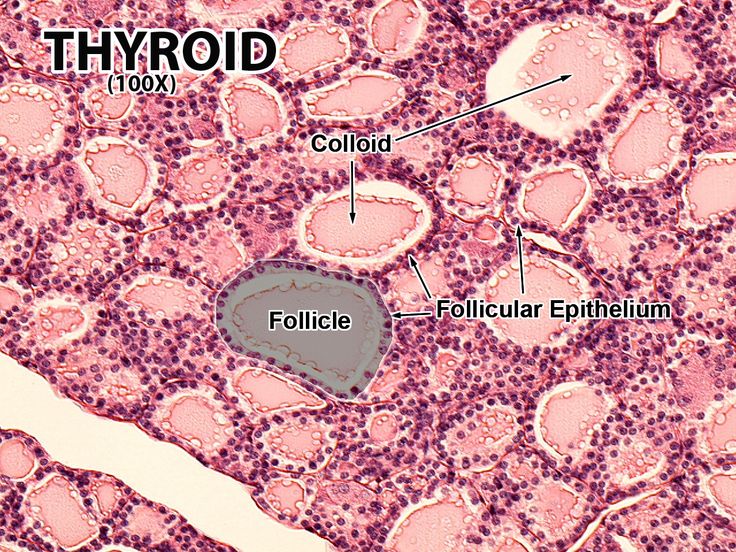
Microstructure
The thyroid gland has a thin capsule of connective tissue, which extends into the glandular parenchyma and divides each lobe into irregularly shaped and sized lobules. The functional units of the thyroid are follicles, which are spherical and cyst-like, between 0.02 and 0.9 mm in diameter. Follicles consist of a central colloid core surrounded by a single-layered epithelium resting on a basal lamina (Fig. 29.23).
Colloid consists almost entirely of an iodinated glycoprotein, iodothyroglobulin, which is the inactive, stored form of the active thyroid hormones, tri-iodothyronine (T3) and tetra-iodothyronine or thyroxine (T4), and is produced by the follicular epithelial cells. Sufficient iodothyroglobulin is stored extracellularly within follicles to regulate the metabolic activity of the body for up to 3 months. Follicles are surrounded by a delicate connective tissue stroma, containing dense plexuses of fenestrated capillaries, extensive lymphatic networks and sympathetic nerve fibres that supply the arterioles and capillaries. Some nerve fibres end close to the follicular epithelial cells.
Follicular cells Follicular cells vary from squamous or low cuboidal to columnar, depending on their level of activity, which is controlled mainly by circulating hypophysial thyroid-stimulating hormone (TSH, thyrotropin). Resting follicles are large and lined by squamous or low cuboidal epithelium with abundant luminal colloid. Apical microvilli are short in resting cells, but elongate and often branch on stimulation by TSH. Follicles showing differing levels of activity may coexist. Active follicular cells are highly polarized functionally. The secretion of TSH leads to endocytosis of colloidal droplets at the luminal epithelium (see Fig. 29.23). The hormone provokes the cells to extend cytoplasmic processes into the luminal colloid and sequester droplets of colloid. The iodinated thyroglobulin in the intracellular colloid droplets is then degraded by follicular cell lysosomes, liberating T3 and T4,
which pass to the base of the cell, where they are released. They are exported from the thyroid mainly via the blood capillaries and lymphatics. Prolonged high levels of circulating TSH induce follicular cell hypertrophy, progressive resorption of colloid and increased stromal vascularity, and this can result in thyroid enlargement. C cells Thyroid parenchyma also contains C (clear) cells, so called because they have pale-staining cytoplasm, which is more pronounced in some species than in the human thyroid. C cells are members of the amine precursor uptake and decarboxylation (APUD) system of dispersed neuroendocrine cells. They produce the peptide hormone calcitonin (thyrocalcitonin), which lowers blood calcium by inhibiting bone resorption and calcium recovery from renal tubule ultrafiltrate. C cells populate the middle third of each lateral lobe of the thyroid and are typically found scattered within thyroid follicles, lying inside the basal lamina but not reaching the follicle lumen. Occasionally, they occur in clusters in the interfollicular stroma, which is why they are also called parafollicular cells.
Thyroidectomy
Apart from variable enlargement during menstruation and pregnancy, any thyroid swelling is a goitre, which may press on related structures. Symptoms most commonly are the consequence of pressure on the trachea or the recurrent laryngeal nerves, and there may also be venous engorgement. During thyroidectomy, care must be taken when tying off the superior and inferior thyroid arteries to avoid damage to adjacent nerves. The external laryngeal nerve runs close to the superior thyroid artery, and the recurrent laryngeal nerve runs close to the inferior thyroid artery. Total thyroidectomy may be necessary for the treatment of hyperthyroidism (overactive thyroid), as well as for thyroid enlargement in the euthyroid state. The parathyroid glands and the recurrent laryngeal nerves are preserved.